A variety of bone graft materials can be utilized in veterinary dentistry. Some of the more common applications for these products include placement in certain extraction sites to help prevent alveolar ridge loss, during surgical periodontal therapy, for fracture repair and to help stabilize near-fractures caused by dental disease. Because of the high degree of hype and misinformation surrounding these materials, I will provide references for some of my comments.
A number of terms have been used in a confusing and overlapping fashion to describe, criticize and promote the use of some of these materials. Would you rather use “glass shards” or a “bi-phasic ceramic bone allograft” for your patients? Me too. Some of these terms, along with their (simplified) definitions include:
- Sintering – a manufacturing process by which two or more different powdered materials are fused into a single solid substrate by heating them to a temperature that is actually below their melting points.
- Ceramic – an inorganic non-metallic solid material produced by heating and then cooling. Some sintered materials are also ceramics and vice versa.
- Bioglass – A material comprised of silicon, sodium, calcium and phosphorous oxides. When implanted, they form a layer of hydroxyapatite-type material on their surface, conducive to osteoblast attachment. Most of these materials have little or no long-term resorption in the body. Artificially produced graft materials, such as bioglass, are terms Alloplastic graft materials.
- Hydroxyapatite (HA) – a crystalline material that is made up primarily of calcium and phosphorous. HA can be produced artificially or naturally, is biologically stable and is not resorbed over time. Normal bone consists of approximately 50% HA.
- Tricalcium Phosphate (TCP)– A ceramic material made of calcium and phosphorous. TCP has been used as a bone graft material alone or mixed with a variety of other products, such as HA, bioglass or bone. When used alone it has poor mechanical stability in the graft site. It is thought to contribute calcium and phosphorous ions for new bone production and some forms of TCP have been shown to have osteo-inductive capabilities (see below).
- Bone Morphogenic Proteins (BMP)– A class of proteins that induce mesenchymal cells to become osteoblasts and even form bone in non-bony sites. BMP activity is highly desirable in graft materials and is present in demineralized freeze-dried bone graft (DFBG).
Until recently, a relatively limited selection of materials were available specifically for the veterinary marketplace. Some exciting new products have been introduced recently, specifically for our patients. This article will cover the spectrum of materials reasonably available for veterinary patients. Please recognize that dozens of other products are available on the human side, but tend to be cost prohibitive for our patients.
Graft materials can have different modes of action, with some being more desirable than others. These can be described as follows:
- Osteoconductive (aka-osteopromotive) – all materials show at least this level of activity, implying they provide a friendly environment for osteoblasts to proliferate and form new bone as they are “conducted” across the graft material. This is the lowest level of activity in graft materials. Bio-glass products and some other artificial materials provide this level of action. Artificial graft materials are termed alloplastic products.
- Osteoinductive – This level of activity is very desirable and means that the product is capable of stimulating undifferentiated mesenchymal cells, present in all tissues, to differentiate into osteoblasts capable of new bone production. There are two different pathways for achieving osteoinduction in graft materials. Some products do this via Bone Morphogenic Protein (BMP) activity. This activity is present in Demineralized Freeze-dried Bone Graft (DFBG). The process of demineralization is thought to unmask proteins present in bone collagen that possess BMP activity. Pure BMP is available experimentally, but is presently cost prohibitive for routine clinical use in veterinary patients. There are also problems with using purified BMP, not the least of which is figuring out how to halt the bone production after it has started. This has led to some unfortunate human fatalities when these materials were utilized for cervical spinal surgery and the patients later experienced uncontrollable progressive compression of the cervical spinal cord. Fortunately, DFBG does not exhibit the problem of uncontrolled new bone growth. This class of materials has exciting possibilities for future dental treatment in veterinary patients, such as regenerating bone in furcation defects and treating horizontal bone loss. More recent evidence has shown that some alloplastic (artificial) graft materials also possess some degree of osteoinduction (ref. 1). The mechanisms of osteoinduction in alloplastic calcium/phosphate ceramics is thought to be different from DFBG and is enhanced when the material has a rough surface, a micro-porous structure and when surrounded by high levels of calcium and phosphorous ions. The osteoinductive pathways of these products result in intra-membranous bone formation, while the BMP pathway leads to endochondral ossification.
- Osteogenic – These products contain live osteoblasts and are capable of producing bone themselves. Auto-grafts harvested from the patient while being treated are an example of this class. While live bone can be harvested from a patient being treated, the cost of the harvesting equipment, increased anesthetic time and patient morbidity at the graft site have limited dental auto-grafts in veterinary medicine. For that reason, this paper will focus on Osteoconductive and Osteoinductive materials.
Veterinary products available in the veterinary marketplace:
Consil(Nutramax) is a synthetic (alloplastic) material made of Bioglass. The human equivalent is sold as “Perioglas”. It comes in a granular and putty form. The putty form is easier to handle but is a little more expensive. After implantation this material forms a hydroxyapatite-like layer on the surface that facilitates osteoblast attachment. Figure 1 shows the structure of a typical Bioglass, which has a very smooth surface. Bone gradually fills in the spaces in between the particles of Bioglass and the material has not been shown to resorb over time.
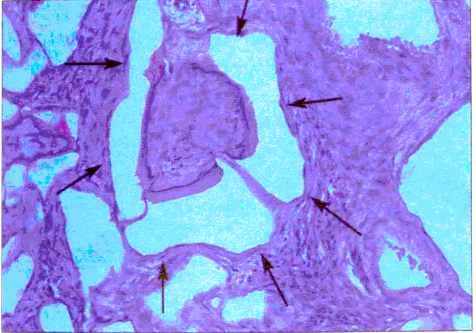
Figure 2. Bioglass after healing. The white areas are the bioglass material and the surrounding tissue in this slide is primarily connective tissue.
The bone that fills in the defect consists largely of the original glass particles (Figure 2). The quality of bone and rate at which the bone is produced around a bioglass has been shown to be highly variable. (ref. 2) Historically this material has been used in extraction sites to help maintain the level of the alveolar bony ridge bone post-extraction and also in periodontal surgery.
Synergy(VTS=Veterinary Transplant Services) is a recently introduced product for the veterinary marketplace (figure 3).
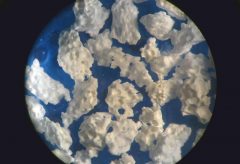
Figure 4. Microscopic structure of Synergy. Note the rough surface concavities and pores in the structure.
It is a alloplastic (synthetic) ceramic graft material consisting of sintered Hydroxyapatite (HA) and Tri-calcium Phosphate (TCP). The sintering process joins the two materials into particles that are rough and porous (figure 4). For comparison, figure 5 shows the similar microstructure of cancellous bone. The rough surface and porosity of the product have been shown to confer osteoinductive properties in similar products. Bone has been shown to fill into the rough surfaces and pores in the product.
Synergy is made primarily of TCP, which eventually dissolves away, gradually opening up more pores in the material into which bone migrates. The HA component provides dimensional stability for the product as the TCP is resorbed and eventually the graft site will consist of mainly normal bone with a small percentage of HA particles. The HA particles in the product are never resorbed. The dissolving TCP is also thought to directly contribute calcium and phosphorous ions for mineralizing new bone. (ref. 3) This material would be appropriate for placement in extraction sites when indicated and as a lower cost alternative in other applications.
Fusion (VTS) has also been introduced recently into the veterinary marketplace (Figure 6). It is a mixture of Synergy (see above) and demineralized freeze-dried bone graft (see below). While not as expensive as pure DFBG, the addition of real bone to the product should provide some osteoinduction via the BMP pathway. This combination of ingredients should provide osteoinduction via two unique pathways. It comes in a putty form and is more expensive than Synergy and less expensive than pure DFBG. This material would be appropriate for a higher quality graft material for extraction sites and near fractures (especially in older patients) or as a lower cost alternative to pure DFBG for use in fractures and surgical periodontal therapy.
Periomix (VTS) is demineralized freeze-dried bone graft (DFBG), available in both canine and feline origins (figure 7). This is the gold standard for pre-packaged bone graft materials in veterinary patients and should be utilized whenever new bone growth is critical. The author uses this material in fracture sites that have bony defects, for near-fractures secondary to dental disease and when performing surgical periodontal therapy with vertical bony defects (open root planing).
Hopefully this will help clear up some of the confusion that exists around these products and help guide rational use of dental bone graft products in your practice.
References
1. Habibovic P, de Groot K Osteoinductive biomaterials-properties and relevance in bone repair. J Tissue Eng Regen Med 2007; 1:25-32
2. Dental implants placed in extraction sites implanted with bioactive glass: Human histology and clinical outcome. Norton R., Wilson J. Intl Journal of Oral and Maxillofacial Implants. 17:2, 2002, pp. 249-257
3. In vivo behavior of two different biphasic ceramic implanted ion mandibular bone of dogs. Farina N, Guzon F. et al. J Mater Sci: Mater Med (2008) 19:1565-1573