 A variety of techniques may be utilized for the treatment of mandibular fractures. Intra-oral splints provide an excellent option for repair of many mandibular fractures, are relatively inexpensive, provides immediate post-operative function, and minimizes the risk of iatrogenic damage associated with other methods of stabilization.
A variety of techniques may be utilized for the treatment of mandibular fractures. Intra-oral splints provide an excellent option for repair of many mandibular fractures, are relatively inexpensive, provides immediate post-operative function, and minimizes the risk of iatrogenic damage associated with other methods of stabilization.
The lower jaw consists of two mandibles, joined together rostrally at the symphysis. The symphysis is not a bony union but rather is joined by a fibrocartilaginous pad. This fibrocartilaginous pad is seen on a radiograph as a radiolucent space and is sometimes misdiagnosed as a fracture.
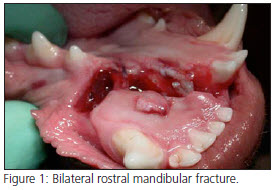
 Mandibular body fractures are common (Fig. 1) and can be classified as being either favorable or unfavorable. The muscles that close the mouth insert on the ventral aspect of the caudal mandible, while the muscles that open the mouth insert on to the ventral aspect of the rostral mandible. A “favorable” fracture is defined as a fracture where the fracture line is directed from the dorsal mandible in a ventral rostral direction. In these cases when the mouth is opened or closed the forces generated by the muscles tend to reduce the fracture. If the fracture line is directed from the dorsal mandible directly ventrally (transverse fracture) or ventral caudally, the fracture is considered to be “unfavorable”. With this type of fracture, when the mouth is opened or closed the forces generated by the muscles tend to pull the fracture line apart. In general, unfavorable fractures require more stabilization than do the favorable fractures.
Mandibular body fractures are common (Fig. 1) and can be classified as being either favorable or unfavorable. The muscles that close the mouth insert on the ventral aspect of the caudal mandible, while the muscles that open the mouth insert on to the ventral aspect of the rostral mandible. A “favorable” fracture is defined as a fracture where the fracture line is directed from the dorsal mandible in a ventral rostral direction. In these cases when the mouth is opened or closed the forces generated by the muscles tend to reduce the fracture. If the fracture line is directed from the dorsal mandible directly ventrally (transverse fracture) or ventral caudally, the fracture is considered to be “unfavorable”. With this type of fracture, when the mouth is opened or closed the forces generated by the muscles tend to pull the fracture line apart. In general, unfavorable fractures require more stabilization than do the favorable fractures.
 The goals of mandibular fracture repair are two fold: Restoration of normal or acceptable occlusion to allow normal mastication, and avoidance of iatrogenic damage to the roots of the teeth and the large neurovascular bundle in the mandibular canal.
The goals of mandibular fracture repair are two fold: Restoration of normal or acceptable occlusion to allow normal mastication, and avoidance of iatrogenic damage to the roots of the teeth and the large neurovascular bundle in the mandibular canal.
The use of pharyngeal endotracheal intubation substantially improves the surgeon’s ability to monitor the dental occlusion during fracture repair. When the procedure is completed, the hole in the skin created for the endotracheal tube may then be utilized for an esophagostomy feeding tube if desired. If pharyngeal intubation is utilized, the endotracheal tube should be closely monitored to avoid sharp bends and ensure patency of the tube.
Intra-oral splints utilize a combination of wire and acrylic composite to provide stability to the fracture site without invading the bone and soft tissue. There are two different acrylic splint materials that are commonly used. The first is Jet Acrylic. Two major disadvantages with this product are the toxic fumes that are created during the mixing process and the damaging heat generated by the exothermic curing reaction. The superior acrylic materials are cold cure composites, “Maxi-Temp” or “Protemp Garant.” When the teeth are properly prepared, acrylics bonds fairly well to the teeth. Ideally there should be at least two teeth with adequate crown surface area rostral and caudal to the fracture site. The addition of inter-dental wire provides substantial improvement in splint strength and retention.
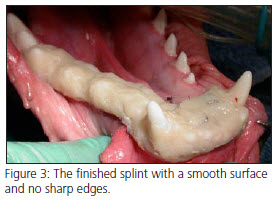
The fracture site should first be carefully cleaned and necrotic material removed. Debridement of the soft tissues should be conservative to help maintain vascular supply. Small bony fragments that are detached or do not contribute to the repair should be removed. Any mobile or severely periodontally compromised teeth near the fracture should be extracted. The site is lavaged and the soft tissues are closed with absorbable suture material. All of the teeth are then scaled and polished. Teeth included in the splint should are polished with flour pumice, since standard dental polishing compounds can interfere with the bonding of the splint material to the teeth. The wire is then placed and tightened. During wire placement, the occlusion should be continually checked to ensure that the teeth line up correctly and that the patient can completely close their mouth. The loops of the twisted wire are placed on the lingual aspect of the mandible, which allows for complete closure of the mouth and normal mastication. Any interference between the arcades should be addressed and eliminated. Achieving functional atraumatic occlusion after repair is more important for healing than is perfect bony reduction. The teeth that will be included in the splint are then acid etched to enhance retention of the composite material. The acrylic is then placed over the teeth and wire. Immediately after placing the acrylic, the mouth should be closed into complete occlusion and held there until the splint material is completely set. (Fig. 2) After the acrylic is set, any sharp edges and rough surfaces are smoothed to minimize soft tissue damage and food retention. (Fig. 3) In unfavorable fractures, interfragmentary or cerclage wires may be added for additional stabilization.
Pain medication is dispensed and antibiotics are frequently indicated to prevent complications in the healing process. Follow up care includes soft food and no toys until the splint is removed. The splint should be brushed twice daily to remove food debris, followed by application of chlorhexidine oral rinse. An Elizabethan collar is occasionally required to prevent self trauma and loosening of the splint. The splint should be rechecked for initial stability in 7-10 days and then radiographed in 4-6 weeks, depending on the fracture and age of the patient. After radiographic evidence of bony healing is evident, the splint is removed. Soft tissue ulceration will be evident after splint removal, but will heal very quickly.
