In response to last month’s newsletter, I received a question regarding the clinical significance of periapical radiographic lesions. The doctor who contacted me was under the impression that the presence of a radiographic periapical lesion might be a contraindication for endodontic (root canal) therapy, and that the PAL represented an area of infected bone (osteomyelitis). Let’s take a look at PAL, what they represent, and their implications for treatment planning.
Below is the radiograph from last month, from an endodontically infected tooth. A classic periapical lucency can be seen around the distal root. For comparison, the second X-ray is from the contralateral tooth in the same patient, showing normal anatomy.
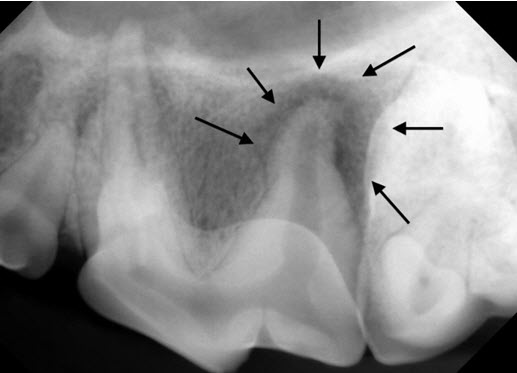
Dental radiograph of 208, showing a large lucent area surrounding the distal root.
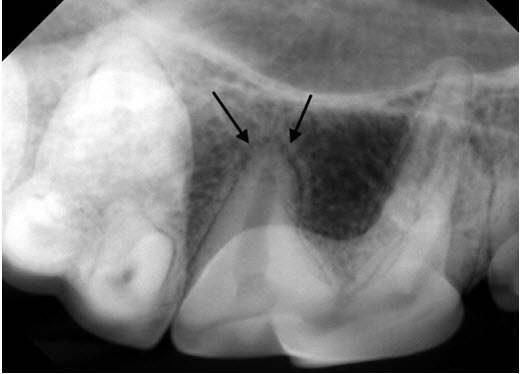
For comparison, the dental X-ray taken of the same tooth on the other side shows the normal appearance of the bone and periodontal ligament space around the back root (arrows).
What do PAL represent? PAL are radiographic signs of demineralized bone, not infected bone. There is frequently granulation-type tissue in the area. These radiographic lesions typically lag behind the disease process, and many non-vital teeth and endodontically infected teeth, while painful, may never show any obvious radiographic signs. This is because PAL do not show up until around 60% of the thick cortical bone of the maxilla or mandible (not the alveolar/socket bone) is demineralized. With the excellent blood supply in the area, true osteomyelitis is pretty rare in the oral cavity. So what you are typically seeing is demineralized bone, not infected bone. PAL may even form without any bacterial infection being present.
Why does this happen? When a tooth becomes non-vital (dies), whether or not they are infected, the necrotic pulp tissue begins to break down inside the tooth. Some of this material begins to leak out around the apex of the root through the small apical delta canals that extend from the end of the root canal to the outside of the root. If you look below at the final X-ray from the past newsletter, you can see the cement highlighting some of those canals, leading to the puff of cement (arrow) on the X-ray. As these materials leak outside the root, they elicit an inflammatory response in the periapical tissues. The presence of bacteria hastens this process. The end result is demineralization of the bone secondary to chronic inflammation.

Final X-ray after root canal therapy. Some faint white lines of cement can be seen leading from the filling material inside the root to the cement “puff” indicated by the arrow.
The problem for the body is that it cannot send white blood cells or blood vessels inside a dead tooth to clean up infection and/or debris. The root canal system is a hiding place, inside the tooth, for the necrotic debris and/or infection. The continual leakage of inflammatory materials from this hiding place, not the PAL, is the primary problem. Think of a splinter or grass awn in a draining tract. Get rid of the splinter or awn and the draining tract heals up. Get rid of the hiding place for debris and/or infection inside the tooth and the body does just fine, probably even without the use of antibiotics. Root canal therapy, done carefully, gets rid of the hiding place for infection and necrotic debris inside the tooth and seals all the little apical delta canals with cement. Once you eliminate the chronic drainage of inflammatory materials from inside the root canal system, the body can clean up the mess surrounding the apex of the root.
There are some limits to what can be done. If the anatomy of the apex is totally obliterated from chronic inflammation, this makes cleaning and sealing the canal more difficult, but still not impossible. In some cases, after obturating the canal with the radio-opaque filling materials it becomes apparent that the apex of the tooth is severely damaged. In some of these cases, we immediately proceed to a short surgical procedure to remove the necrotic section of the apex. This is rare. If the apical 1/3 of the root is severely damaged from chronic inflammation, that tooth is a poor candidate for treatment.
In a case such as the one presented in the last newsletter, I typically send them home on 10 days of antibiotic therapy, usually Clindamycin or Clavamox. The need for this antibiotic therapy is questionable. The main thing is getting rid of the hiding place for necrotic tissue and/or infection inside the tooth. Again, think of the splinter analogy. If infection in the bone was the main problem, then simple extraction of the tooth, which is almost always curative, would not suffice.
These cases are followed radiographically to ensure success, looking for progressive resolution in the PAL. We typically like to see follow-up dental radiographs in the 6-12 month range and annually therafter. In some cases, PAL can heal with scar tissue in the periapical area, which would keep the radiographic PAL from totally resolving. We are starting to split hairs here, but in my mind if I see progressive resolution of most of the PAL over time, I am OK with a small lucent area near the apex that does not completely resolve. Failed cases are characterized by very minimal to no radiographic improvement. As in all aspects of medicine, some cases fall into a grey area.
Bottom line – PAL in and of themselves, are not a contraindication to successful root canal therapy. I have treated hundreds of cases with PAL that have resolved successfully. There is one published veterinary study on success of root canal therapy in veterinary patients. They showed decreased success in root canal therapy in teeth with pre-operative PAL. This may be partially due to the grading criteria used to define success. I have treated hundreds of cases with PAL that have resolved successfully.
