This month’s case is interesting in that it involved treatment of a right lower canine tooth (404) that had been treated seven years previously with vital pulp therapy. The patient had initially presented at 10 months of age for treatment of base-narrow lower canine teeth (BNMCT). For a more complete discussion on all the options for treatment of base-narrow canine teeth, please see the archived versions of the January, February and March 2012 newsletters. This three-part series is a complete review of the pathology, options for treatment and techniques used by the author to treat this very common malocclusion. Many of the techniques used to treat BNMCT are well within the grasp of a general practitioner.
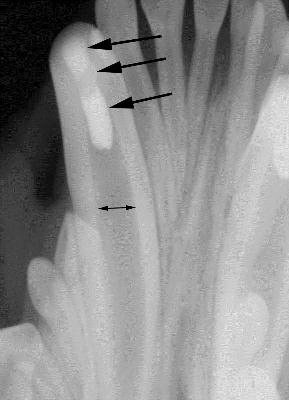
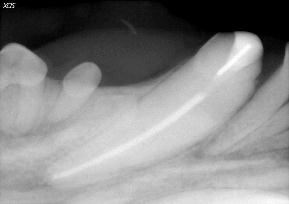
To maintain function, the best option for the initial treatment in this patient was determined to be crown reduction and vital pulp therapy (aka-“pulp cap”), which was performed. Figure one is a radiograph prior to the initial treatment, showing the wide root canal spaces that were present in the patient at that time (arrows). One reason vital pulp therapy was chosen for this patient is that, properly performed, the tooth remains vital, allowing the immature tooth to continue to mature and strengthen through the continued deposition of secondary (physiologic) dentin. Figure two is a post-op-radiograph showing the three layers of the restoration (MTA, glass ionomer and composite). Periodic follow-up radiographs on this patient had shown the lower canine teeth to be vital with continued maturation.

Figure one, showing the wide root canals present in young patients.
Seven years after initial treatment, the patient presented with an oblique complicated crown/root fracture of 404, which was of unknown etiology and duration. A complicated fracture is one that involves the root canal system of the tooth. The fracture extended under the gingival margin in an oblique fashion and the root canal could be clearly seen in the fracture site. Figure three shows the initial radiograph. Due to the geometry of the radiograph, the oblique nature of the fracture is not readily apparent.
The width of the root canals of both lower canine teeth are seen to much narrower when compared to the radiographs taken at the time of the initial treatment and fairly equal to one another, indicating that both of these teeth had remained vital (alive) and continued to mature. The apex of 404 is seen to be substantially shorter than the apex of 304 and 404 has a large periapical lucency. These finding would indicate that the fracture had been present for some time, leading to lytic changes and loss of apical root structure in 404 secondary to bacterial infection. Figure four shows an occlusal view of the fracture and Figure five shows a lateral view of the fracture. The oblique nature of the fracture can be appreciated. When the root canal system is exposed in a mature tooth, the best options for treatment are either root canal therapy or extraction of the tooth. The owner preferred to maintain as much function as possible and avoid the trauma of extracting a mandibular canine tooth.
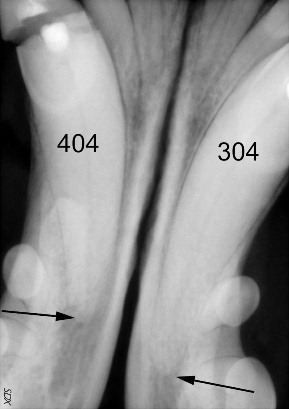
Figure three, showing the apical lysis of 404 compared to 304. Tooth 304 has a small dark periapical lucency (arrow) that is actually the middle mental foramen, a normal anatomic structure usually located below the mesial root of the second premolar.
The mesial fracture fragment was removed. Figure six shows the fracture fragment. The layer of MTA that was initially placed is visible, as is the layer of reparative dentin that had formed underneath the MTA. Formation of reparative dentin under the MTA is the goal when performing vital pulp therapy. At the time we initially treated with patient, only gray MTA was available. We now use MTA that is white colored, which eliminates the gray staining of the crown of tooth after treatment. Figure seven shows the fragment completely removed, with a periodontal probe placed into the fracture site and coming out the draining tract of the periodontal abscess that had formed at the mucogingival line.
Figure 8. Shows the final result. The tip of the retention pin is barely visible in the center of the composite restoration. Figure 9. Shows a final radiograph after treatment. The pin is clearly visible in the composite restoration and a small amount of extruded cement (“puffs”) can be seen around the apex of the tooth. In the author’s opinion, the puffs are an excellent indicator of adequate obturation of the canal. The cement is usually completely gone on follow-up radiographs.
After removal of the fragment, a surgical periodontal flap was made to gain access to the fracture site, several small fracture fragments were removed and root canal therapy was performed. The damaged areas of the surrounding bone was then contoured to a normal shape and de-mineralized freeze-dried bone graft was placed into a vertical bony defect created by the fracture. The crown was then restored to a more normal shape with composite restorative material, utilizing a small pin placed in the dentin. The pin provides additional retention for the composite restoration, allowing more complete restoration of the crown. The final step was suturing the periodontal flap carefully around the tooth, taking care to surround the entire tooth with a collar of attached gingiva.
This case illustrates several interesting points. It shows the desired outcome of vital pulp therapy and illustrates the importance of follow-up radiographs to ensure that teeth treated with vital pulp therapy remain vital and continue to develop. It also shows that many fractured teeth can be restored with available periodontal and restorative techniques. The goals of treatment for this patient were to avoid a traumatic extraction, to maintain adequate crown height to help keep the patient’s tongue in the mouth when panting and to allow continued function of the tooth for picking up and holding objects in the mouth. Additional crown height could have been achieved either with a larger pin placed further down into the root canal space or by placement of a crown on the tooth. The restorative solution utilized for this patient was completed in one visit and met the treatment goals stated.